Rheumatoid Arthritis

WHAT IS RHEUMATOID ARTHRITIS?
Rheumatoid Arthritis (RA) is a chronic autoimmune inflammaory disease. The cause of RA is unknown1.
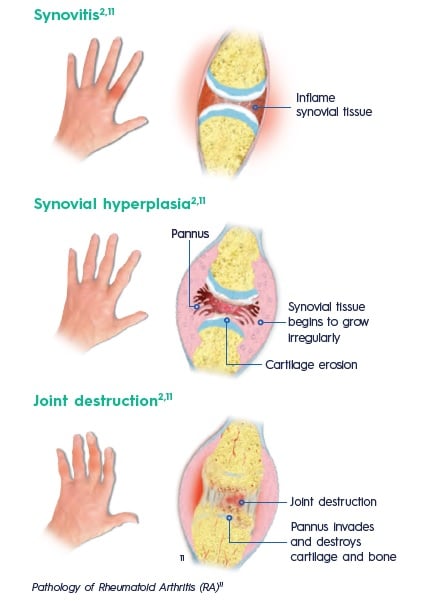
In a joint with RA, the lining of the joint becomes inflamed causing damage to joint tissue. This tissue damage can cause long-lasting or chronic pain, unsteadiness and deformity.
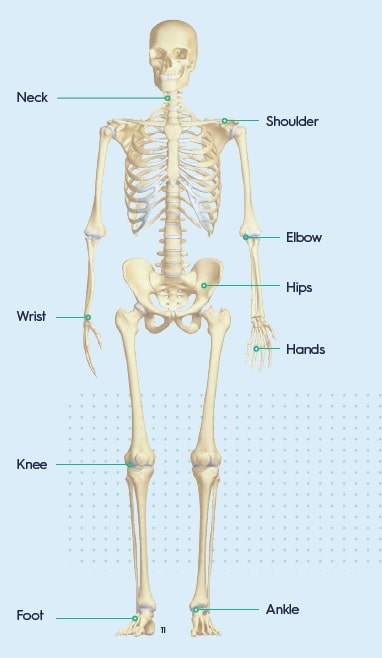
WHICH JOINTS ARE AFFECTED BY RA?
RA mainly attacks the joints, usually many joints at once, but it can also affect other parts of the body1,3.
Joints that may be affected include4:
WHAT ARE THE SIGNS AND SYMPTOMS OF RA?
With RA, there are times when symptoms get worse, known as flares, and times when symptoms get better, known as remission1.
In most cases, symptoms come on gradually3:
Early symptoms1,2,4
- Fatigue
- A low-grade fever
- Weight loss
- Swollen and tender joints
- Morning stiffnes
Early RA tends to affect smaller joints first, particularly hands and feet. As the disease progresses, symptoms often spread to the larger joints such as wrists, knees, ankles, elbows, hips and shoulders4,5.
WHAT ARE THE CAUSES AND RISK FACTORS FOR RA?
Although the specific cause of RA is not known there are some factors that can increase the risk of developing the disease1:
- Age. RA can occur at any age, but the risk increases with age. The onset of RA
is highest among adults in their sixties1. - Gender. Women are affected two to three times more often than men2.
- Genetics/family history. A family history of RA increases the risk to developing the disease three to five times2.
- Cigarette smoking1,6
- History of live births. Women who have never given birth may be at greater risk of developing RA1.
- Stress. Some people report emotional stress or trauma before the onset of RA6.
- Obesity. Being obese can increase the risk of developing RA. The more overweight a person is, the higher the risk of developing RA1,6
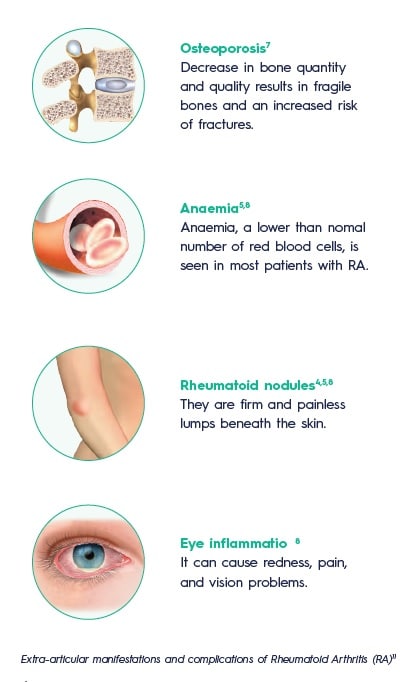
WHAT ARE THE COMPLICATIONS OF RA?
During the clinical course of RA, up to 40% of people may develop extra-articular manifestations5:

HOW WILL MY DOCTOR DIAGNOSE MY DISEASE?
The diagnosis is based upon multiple factors including8:
- Person’s medical history
- Physical examination
- Results of blood tests
- Results of imaging tests
Signs and symptoms of RA are not specific and can look like signs and symptoms of other inflammaory joint diseases1.
A classification criteria is used as an aid for diagnosis of RA and includes4:
Signs of inflammation in 3 or more joints, lasting for 6 weeks or longer4.
Diagnostic antibody blood tests:
rheumatoid factor and/or anti-citrullinated peptide/protein antibody2,8.
Elevated blood levels of C-reactive protein or the erythrocyte sedimentation rate, markers that reflect the level of inflammation in the body2,8.
Timely and precise diagnosis is of high importance in RA treatment, since early diagnosis can arrest disease in many patients, thereby preventing or slowing disease progression, irreparable joint damage, and disability in up to 90% of RA patients2.
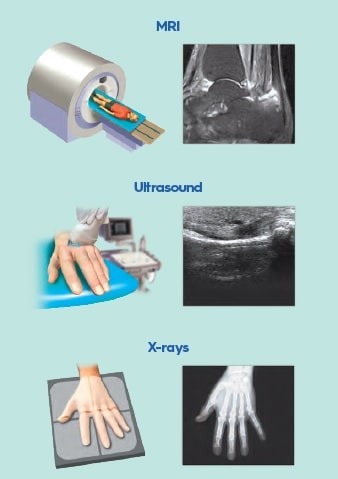
IMAGING TESTS
Even though X-rays are still used as a diagnosis technique of late changes in the joints and to monitor disease progression, it has limitations for early diagnosis of RA9.
Both ultrasound and magnetic resonance imaging (MRI) are recommended for diagnosing and monitoring disease activity in RA patients2.
WHAT ARE THE TREATMENT OPTIONS FOR RA?
The aim of RA treatment is to either reach full remission or at least significantly lower disease activity to control symptoms, prevent joint damage, and maximize patient’s quality of life and ability to function2,8.
The available therapeutic drugs include non-steroidal anti-inflammatory drugs (NSAIDs), immunosuppressive glucocorticoids, and disease-modifying anti-rheumatic drugs (DMARDs). Drug treatment is typically supplemented by non pharmacological treatment which includes physical therapy to sustain joint mobility, patient counselling to slow down disease progression, and surgery in cases of severe stages of RA which provide pain relief and restore the function of joints2,9.
NSAIDs2
- Only symptom improvement (pain and stiffnes ) but no influence on disease progression
- Only used as a symptomatic treatment until diagnosis is established
Non-pharmacological treatment2
- Physical therapy
- Patient counselling (lifestyle, smoking, exercise, ideal body weight, drug adherence)
- Surgery
Glucocorticoids2
- Non-specific immune suppression
- Rapid systemic disease-modifying effects
- But long-term side effects
DMARDs2
- Medicine that interferes with signs and symptoms of RA
- Target inflammation
- Prevent further joint damage
WHAT CAN I DO TO MANAGE MY DISEASE?
There are self-care measures that can help manage the signs and symptoms of RA8:
Exercise regularly5
Exercise and physical activity improve muscle strength and perceived health status.
Apply heat and cold8
Heat treatments can help to relax stiff joints and tired muscles.
Cold is best to reduce pain and inflammation
Stop smoking1
Reduce stress8
There are different ways to relax and stop focusing on pain. They include meditation,
deep breathing, guided imagery and massages.
Healthy dietary habits10
They can be a useful tool in reducing the risk of RA, related comorbidities, RA progression and disease activity. Mediterranean diet is the most encouraged dietary pattern.
Maintain a healthy weight1

