Juvenile Idiopathic Arthritis

WHAT IS JUVENILE IDIOPATHIC ARTHRITIS?
Juvenile idiopathic arthritis (JIA) is a heterogeneous group of diseases that affect children under 16 years of age and cause stiff or swollen joints and pain that last 6 weeks or more1,2,3.
TYPES OF JUVENILE IDIOPATHIC ARTHRITIS
The International League of Associations for Rheumatology (ILAR) classifies JIA into seven different types. Although chronic arthritis is mandatory for all types, they have distinct extraarticular and systemic clinical manifestations, genetic predispositions, and disease course2,3:
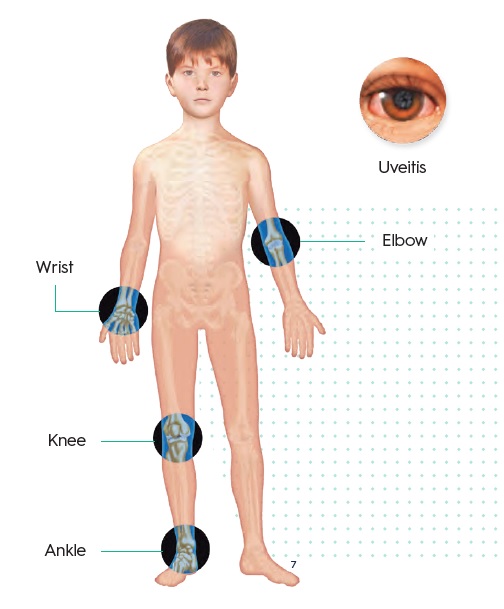
- Oligoarthritis
- Juvenile enthesitis-realted arthritis
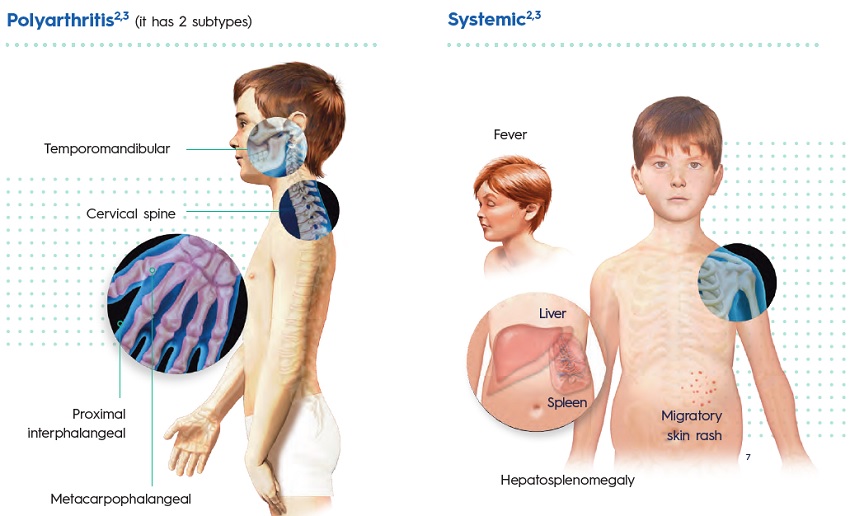
- Polyarthritis (it has 2 subtypes)
- Juvenile psoriatic arthritis
- Systemic
- Others
JUVENILE ENTHESITIS-RELATED ARTHRITIS
Arthritis usually involving the vertebral column, hips and legs.
Metacarpophalangeal
Arthritis affecting 5 joints or more during the first 6 months of disease and:
- Negative test for rheumatic factor (RF- Polyarticular JIA)
- Positive test for rheumatic factor (RF+ Polyarticular JIA)
Hepatosplenomegaly
Arthritis affecting more than 1 joint with, or preceded by, fever of at least 2 weeks of duration. It is accompanied by at least one of the following: skin rash, lymph node enlargement, hepatomegaly and/or splenomegaly, or serositis.
WHAT ARE THE SIGNS AND SYMPTOMS OF JUVENILE IDIOPATHIC ARTHRITIS?
Joint pain, stiffness and swelling1
- The joint symptoms occur in all types of JIA1.
- The joints affected depend on which type of IJA the child has1.
- Some children have a stiiff or swollen joint that does not hurt1.
- Limping4
- Reduced activity level4
- Reluctance to use an arm or leg4
- Dificulty with fine motor activities4
JIA may be difficult to diagnose because some children may not complain of pain at first and joint swelling may not be obvious4.
OTHER SYMPTOMS CAN INCLUDE:
- Fever
It is the most common symptom of systemic JIA. Fever usually occurs daily at the same time for 2 weeks or more1,5. - Rash
It is the second typical extra-articular manifestation in children who have systemic
JIA. The rash is usually described as small salmon pink patches. It occurs with fever spikes but may persist when fever is resolved1,5. - Eye redness (uveitis)
It is the most serious complication for all children with JIA. Uveitis is usually painless, but can lead to vision loss1,5.
WHAT CAUSES JUVENILE IDIOPATHIC ARTHRITIS?
The cause and trigger of JIA remain unclear, as it is not known what causes the immune system to malfunction in JIA2,4.
It is thought that the abnormal immune response is triggered by environmental factors in genetically susceptible individuals2.

There is strong evidence for a genetic component to the aetiology of JIA, being the strongest genetic association with genes of the major histocompatibility complex (MHC), which are central to immunity and and inflammatory processes3,5.
All types of JIA lead to a final common pathway: thickening and inflammation of the joint lining3.
HOW WILL MY DOCTOR DIAGNOSE MY DISEASE?
Physical exam and medical history
Diagnosis of JIA based on physical exam and medical history4. The following items are essential for diagnosis and classification of JIA2:
- Age of onset
- Affected joints
- Duration of arthritis
- Associated symptoms or diseases
- Physical and musculoskeletal examination
Laboratory tests
Chlidren often test negative for blood tests that are commonly found in adults with rheumatoid arthritis such as rheumatoid factor (RF)4. Other inflammatory markers evaluated are2:
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP)
- Human leukocyte antigen (HLA)-B27
Imaging
Imaging serves to improve the certainty of a diagnosis of JIA and to evaluate joint damage2.
- X-rays
- Ultrasound (US)
- Magnetic resonance imaging (MRI)
WHAT ARE THE TREATMENT OPTIONS?
The best care for children with arthritis is provided by a paediatric rheumatology team that has extensive experience and can diagnose and manage the complex needs of the child and family most effectively4.
Pharmacological treatment
NSAIDs
Non-steroidal anti-inflammatory drugs are the most commonly used medicine in JIA as they have analgesic and anti-inflammatory properties5.
Corticosteroids
When only a few joints are involved, a steroid can be injected into the joint before any additional medications are given. Steroids injected into the joint do not have significant side effects4.
DMARDs
Disease-modifying anti-rheumatic drugs (DMARDs) are added as a second-line treatment when arthritis involves many joints or does not respond to steroid joint injections4. Some DMARDs are known as “biologics”, and all of them may cause side effects that need to be monitored and discussed with the paediatric rheumatologist treating your child1,4.
NON-PHARMACOLOGICAL TREATMENT
Physical and occupational therapies
Physical and occupational therapy can improve children’s quality of life by teaching
them ways to stay active and how to perform daily tasks with ease6
Hot and cold treatments
Heat pads or warm baths are useful for soothing stiff joints and tired muscles.
Cold is useful for acute pain6
WHAT CAN I DO TO MANAGE MY DISEASE?
Children with JIA should attend school, participate in extra-curricular and family activities, and live life as normally as possible4.
Exercising regularly6
- Regular exercise helps ease joint stiffness and pain.
- Low-impact and joint-friendly activities such as walking, swimming, biking and yoga are the best option.
- However, children with well-controlled disease can participate in just about any activity they wish.
Having a healthful diet6
- There is no special JIA diet, but consumption of some foods and avoidance of others may help to reduce inflammation
- Foods to include in your child’s diet: fatty fish, fruits, vegetables, whole grains and extra virgin olive oil among others.
- Foods to avoid: high-fat, sugary and processed foods.
Balancing activity with rest6
- When JIA is active it is important to balance light activity with rest.
- Rest helps reduce inflammation and fatigue.
- Taking breaks throughout the day protects joints and preserves energy.
Managing stress and emotions6
- Children and teens with JIA are more likely to get depressed because they are living with a chronic disease.
- It is important to have a strong support system of friends and family that can provide emotional support during tough times.


Related Brochures

crohns-disease

joints
