Ankylosing Spondylitis

What is Ankylosing Spondylitis?
Ankylosing spondylitis (AS) is a chronic inflammatory disease that cause pain and stiffness in the back, neck and sometimes in other joints such as the hip and heels1.
AS begins with inflammation around the bones in the spine or some joints, and later, it can sometimes cause the bones in the spine to fuse together, resulting in the loss of flexibility and the fusion of the spine, resembling “bamboo” with an immobile position1,2.
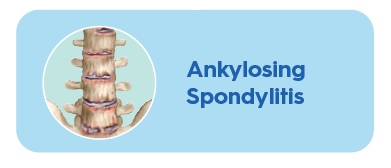
WHICH JOINTS ARE AFFECTED BY ANKYLOSING SPONDYLITIS?
Frequency of inflammation per region6
WHAT CAUSES ANKYLOSING SPONDYLITIS?
AS is an inflammatory disease of unknown aetiology, with a higher incidence in young males2,3. As an autoimmune disease, AS develops through complex interactions between genetic background and environmental factors2.
Genetic background
AS is associated with the presence of the allele HLA-B27.
In fact, 90-95% of AS patients are HLA-B27 positive2.
Environmental risk factors
But AS does not develop in every person who is HLA-B27 positive; thus, it is clear that environmental factors are important. Even first-degree relatives who
are HLA-B27 positive do not uniformly develop the disease2.
ASIDE FROM GENETICS, OTHER FACTORS ARE THOUGHT TO BE INVOLVED:
- Intestinal microbiome: up to 70% of patients with AS have subclinical intestinal inflammation, suggesting that the origin of the disease may be in the gut
- Infections
- Mechanical stress
- Changes in the immune system
- Gender
WHAT ARE THE SYMPTOMS OF ANKYLOSING SPONDYLITIS?
The course of AS and its onset varies greatly from person to person, but symptoms generally start to appear in late adolescence or early adulthood (between 17 and 45 years old)5.
The most common symptom is pain in the lower back and buttocks. This pain usually5:

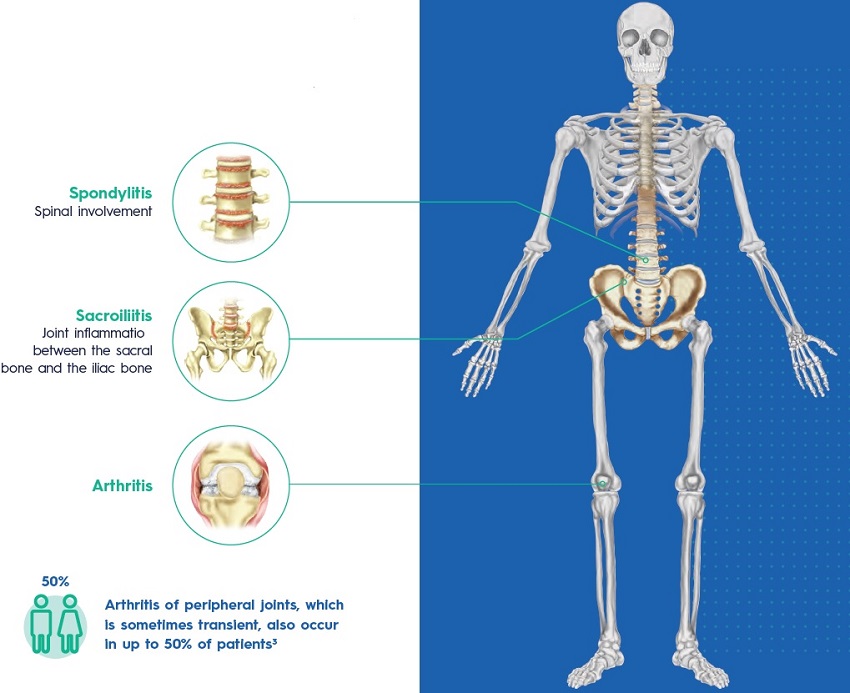
OTHER MANIFESTATIONS OF ANKYLOSING SPONDYLITIS
Extra-articular involvement
Extraskeletal organs may also be affected by this disease. The most common extraarticular manifestations of AS include7:
>50% Inflammatory bowel disease
25% to 35% Acute anterior uveitis
-10% Psoriasis
AS is also associated with7:
- An increased risk of cardiovascular disease.
- Pulmonary complications as diminished chest wall expansion and decreased spinal mobility predispose patients to a restrictive pulmonary pattern.
HOW WILL MY DOCTOR DIAGNOSE MY DISEASE?
AS is diagnosed based upon the recognition of a pattern of clinical, laboratory, and imaging finding characteristic of the disease8,9.
- Physical examination9
Assessment of your flexibility and joint tenderness. - Blood test to look at inflammatory markers8,9
C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) can be assessed in patients suspected of AS. - Blood test which can identify if you carry the HL-B27 gene9
- X-rays9
X-rays will show if there have been any changes to your bones and joints such
as extra bone growth or fusion. - Magnetic resonance imaging (MRI) fusion9
MRI will show if there is any inflammation around your joints.
WHAT ARE THE TREATMENT OPTIONS?
Treatment depends on your symptoms and how severe your condition is1.
The goal of treatment is1:
- To relieve your symptoms
- To help you do your normal activities
- To keep your condition from causing other problems
Non-pharmacological interventions2,10
- Patient education
- Exercises and physical therapy
- Smoking cessation
The use of a biologic agent for AS is particularly appropriate for those with high or very high disease activity, although they are effective in patients with mild to moderate symptoms as well10.
PHARMACOLOGICAL TREATMENT
Nonsteroidal anti-inflammatory medications (NSAIDs)
In many patients, NSAIDs are the only medications required as they are efficient in alleviating AS symptoms in 70-80% of patients.
Biologic therapy
Tumour necrosis factor (TNF)-α inhibitors. TNF inhibitors are recommended for patients with an inadequate response to initial therapy with NSAIDs.
Interleukin (IL)-17 inhibitors. In patients who have contraindications to the use of TNF inhibitors, treatment with IL-17 inhibitors is recommended.
Glucocorticoids
Local injections of glucocorticoids into the involved joint are an option for treating arthritis as they could provide immediate symptom relief.
WHAT CAN I DO TO MANAGE MY DISEASE?
You can reduce the chance that your conditions will cause problems if you1:
- Stop smoking (you will be less likely to have breathing problems)
- Get plenty of calcium and vitamin D (you will keep your bones from getting weak)
- Do exercise (you will prevent some of the stiffnes caused by AS)
- Use a thin pillow (sleeping on a thick pillow can cause neck problems in people with AS)
BENEFITS OF EXERCISE
Increased flexibility
The more flexible you are the easier it is to do everyday tasks.
Increased range of movement
The more mobility you have the easier it is to do things.
Improved posture
Better posture makes you feel better in yourself and reduces feelings of self consciousness.
Improved sleep
Exercise is physically tiring which improves sleep quality, ensuring you wake feeling refreshed.
Reduction in stiffness and pain
Exercise can result in less pain at night and improved sleep quality.
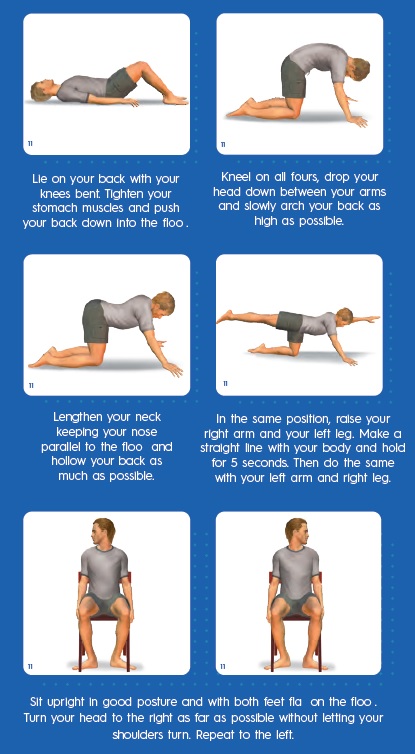
EXERCISES FOR PATIENTS WITH AS
Repeat each of the following exercises at least five times:

Related Brochures

psoriatic-arthritis

arthritis-joint-pain
