Paediatric Inflammatory Bowel Disease

WHAT IS PAEDIATRIC INFLAMMATORY BOWEL DISEASE?
Paediatric inflammatory bowel disease (PIBD) includes Crohn’s disease (CD), ulcerative colitis (UC) and inflammatory bowel disease unclassified (IBDU)1,4.
This medical condition occurs during early childhood (before 16-18 years)1.
PIBD is a chronic, relapsing and remitting inflammatory condition characterised by intestinal inflammation leading to abdominal pain, diarrhoea, bloody stools and other intestinal and extra-intestinal symptoms and complications1.
WHAT IS PAEDIATRIC CROHN’S DISEASE?
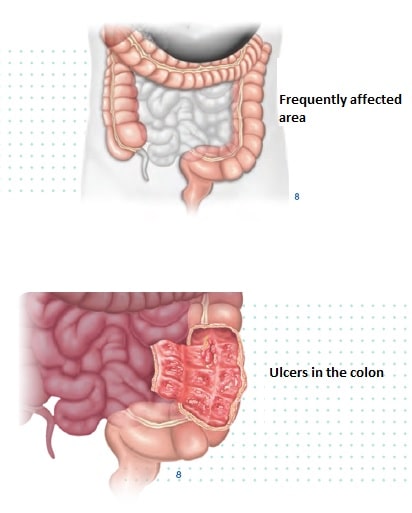
Paediatric CD can affect any portion of the digestive tract from the mouth to the anus. However, it most commonly involves the terminal part of the small intestine (ileum) and the large intestine (colon)2,3.

WHAT IS PAEDIATRIC ULCERATIVE COLITIS?
In Paediatric UC, the inflammation is often limited to the colon, starting from the rectum3,4,5.
WHAT ARE THE SYMPTOMS OF PIBD?
The most common clinical features of Crohn’s disease in children are1:
- Abdominal pain (>85%)
- Diarrhoea (>75%)
- Weight loss (>55%)
The most common clinical features of Ulcerative colitis in children are1:
- Abdominal pain (>85%)
- Bleeding per rectum (>90%)
- Diarrhoea (>90%)
Some affected children may also feel tired, experience fever or loss of appetite. Growth retardation is common at the time of diagnosis, especially in paediatric CD2,5.
EXTRAINTESTINAL MANIFESTATIONS OF PIBD
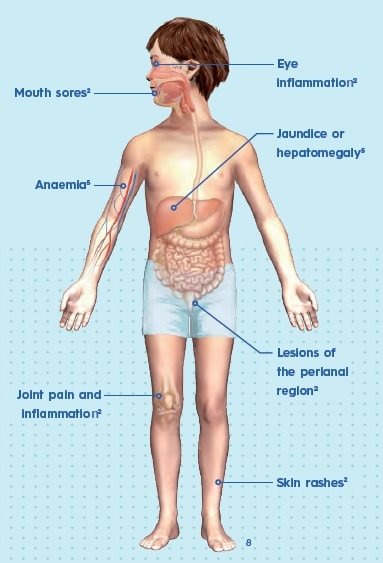
IBD in children also presents with extraintestinal manifestations, which include2,5:
WHAT CAUSES PAEDIATRIC IBD?
The specific cause of paediatric IBD is not fully understood. The disease most likely occurs due to a combination of genetic, immunologic and environmental factors1,2
Genetic predisposition
- Alterations of several different genes play a role in the disease2,3
- Many of the genes associated to paediatric IBD are involved with the function of the immune system2,4,5
- Between 15% to 25% of children with IBD have an affected relative1,2,3
Environmental factors
- Bacterial or viral infections2
- Frequent antibiotic use2
- Westernised diet2
- Smoking2
- Imbalanced gut microbiota2
Paediatric IBD occurs when, in genetically predisposed individuals, the immune system responds to a trigger in an abnormal way. The immune system does not shut off appropriately and mistakenly attacks the small and large intestines leading to chronic inflammation.
HOW WILL THE DOCTOR DIAGNOSE MY CHILD’S DISEASE?
Doctors can do the following tests2,3,5:
Blood tests To check for anaemia (low level of red blood cells) and inflammation (high level of white blood cells)2.
Colonoscopy Doctors put a thin tube with a camera into the rectum to allow the view of the entire colon. It also allows doctors to remove a small sample of tissue (biopsy) to detect microscopic inflammation2,5.
Stool tests To check for infection and hidden blood within the digestive tract2,3.
Endoscopy Similar to a colonoscopy, the tube is inserted down the throat allowing the examination of the upper portion of the digestive tract2.
Imaging tests X-rays, CT scans or MRI scans. Imaging test show pictures of the inside of the body2.

WHAT ARE THE TREATMENT OPTIONS FOR CHILDREN?
There is no cure for CD and UC, but with proper treatment and support, the disease can be effectively managed and may go into remission for long periods of time. Affected children can lead fairly normal lives2.
Treatment options include medications, nutritional and diet therapy, and surgery2.
MEDICATION
Medication for CD and UC in children aim to reduce inflammation2.
- Aminosalicylates: used to treat mild or moderate disease2,6.
- Corticosterioids: stronger anti-inflammatory drugs to treat moderate or severe disease2,6.
- Inmunomodulators: used as maintenance therapy for severe cases2,6.
- Biologics: are complex molecules that are produced in living organisms. They function in preventing inflammation and inducing mucosal healing. Biologics include anti-TNF-α (Tumor Necrosis Factor alpha) monoclonal antibodies such as inflixima, among others like adalimumab and certolizumab pegol2,3.
SURGERY
It is recommended when other therapies have not worked2,3. Doctors can:
- Remove diseased tissue: after surgery, most people are still able to have bowel movements as usual, through the anus3.
- Reopen a part of the digestive system that is blocked2
NUTRITIONAL THERAPY
- Enteral nutrition: involves consuming all calories from a special formula instead of regular diet2.
- Micronutrient deficiencies: your child may require vitamin supplements to maintain their nutritional needs1,3.
WHAT CAN CHILDREN DO TO MANAGE THEIR DISEASE?
Avoid food that might worsen your symptoms
There are foods that doctors may recommend avoiding because they are difficult to digest and could worsen your symptoms. These foods include popcorn, uncooked vegetables, milk, nuts and certain spices2.
Take dietary supplements Disease factors that include chronic blood loss, intestinal malabsorption, decreased intake, and chronic inflammation place children with CD and UC at risk for deficiencies of various micronutrients, such as iron, folate, vitamin B12 and vitamin D3.
Avoid taking NSAIDs Anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can have an adverse effect on the disease7
Seek counselling or join a support group
Up to 25% of adolescent patients with IBD may have symptoms of depression that often are undetected. Psychological support is highly encouraged for families affected by paediatric IBD, especially for the patients, to provide strategies for coping with a chronic disease long term. Cognitive behavioural therapy is a useful tool in treating depression and anxiety5
Getting screened for colon cancer
Due to chronic inflammation, patients with UC and CD involving the colon have an increased risk for colon cancer. The risk increases with time from diagnosis, higher-risk groups include those younger at diagnosis. This might mean having a colonoscopy with surveillance biopsy every 1 to 2 years starting about 8 years after the diagnosis3


Related Brochures

crohns-disease

juvenile-idiopathic-arthritis
